Background: Sickle cell disease (SCD) is an inherited disorder that can cause a range of clinical complications, featured by unpredictable and recurrent acute painful episodes associated with vasoocclusive crises (VOCs). Individuals with SCD experience frequent VOCs and require high doses of opioids for pain control. Thus far, studies on biomarkers associated with VOCs in SCD are very limited and the known markers are hardly considered as critical end points in studying VOCs in SCD. This study aimed to comprehensively analyze immune and inflammatory characteristics of patients with SCD to understand the disease-specific pathogenesis and develop targeted diagnostic and therapeutic strategies related to VOCs.
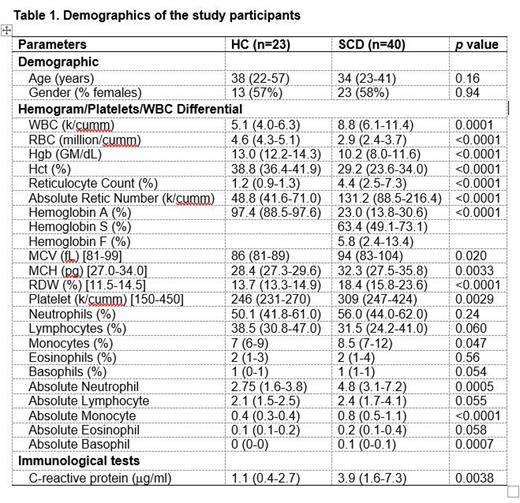
Methods: The study cohort consisted of 40 patients with SCD aged 14-73 years (23 female, 58%), recruited for an ongoing clinical trial (ClinicalTrials.gov Identifier: NCT05045820). Twenty-three ethnicity-, age- and gender-matched pain-free participants were also enrolled as healthy controls (HCs) (Table 1). Multiplex immunoassays were used to profile 80 inflammatory cytokines/chemokines/growth factors and 18 autoantibodies in plasma samples from patients with SCD and the matched HCs. Peripheral blood mononuclear cells were used to profile immune cells. Statistical analysis was performed using GraphPad Prism with Mann-Whitney test, χ 2 test, and Spearman's correlation. P < 0.05 was considered statistically significant.
Results: Patients with SCD exhibited significantly higher plasma levels of 34 analytes, including 12 pro-inflammatory/anti-inflammatory cytokines (IFN-γ, IL-1α, IL-2, IL-8, IL-9, IL-18, TNF-α, TNF-β, IL-4, IL-5, IL-6, and TSLP), 10 chemokines (CCL21, CCL23, Eotaxin-2, Gal-3, GRO-α, IP-10, MCP-2, MIP-1α, MIP-1β, and MIP-3α), 8 growth factors (bNGF, G-CSF, GM-CSF, HGF, IL-7, IL-20, IL-34, and LIF), 2 effectors (granzymes A and B), and 2 soluble receptors (PTX3, TREM-1). Higher activation levels of B cells, CD4 T cells, CD8 T cells, and MAIT cells were seen in patients with SCD. Autoantibody profiles were also altered in patients with SCD, with elevated levels of antibodies against SSA/Ro60, Ribosomal P, Myeloperoxidase, and PM/Scl-100. Levels of cytokines/chemokines/growth factors were correlated with time interval between blood draw and occurrence of VOCs. Four soluble factors (Eotaxin-2, GRO-α, IL-6, and LIF) were positively associated with time interval after VOCs, while two factors (IL-18 and granzyme A) showed negative associations with time interval, suggesting that the altered inflammatory mediators were associated with the occurrence of VOC events.
Conclusion: Our results provide novel and comprehensive understanding of the immune and inflammatory dysregulation in patients with SCD and their relationship with occurrence of VOCs, offering insights into potential SCD-specific biomarkers for further investigation.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal